Abstract

Background: The DEAD-box helicase 41 (DDX41), an RNA helicase, have been described as a component of the RNA spliceosome (Cheah et al. International Journal of Hematology 2017). Although DDX41 mutations predispose to late-onset higher grade myeloid neoplasms (MN), these patients may have a trend toward favorable prognosis and outcomes. In this work, we describe the clinical characteristics and survival outcomes of isolated and co-mutated DDX41 patients (pts).
Methods: We retrospectively analyzed 4,524 consecutive pts who underwent next-generation sequencing (NGS) (OncoHeme 42 genes panel, Mayo Clinic) testing and included 32 pts harboring pathogenic DDX41 mutation and one pt with proven DDX41 germline variant of unknown significance (VUS). Chart review of DDX41-mutated (m) cases between 2009 and 2021 was conducted after IRB approval. We compared overall survival (OS) of unmatched 27 t(8;21)AML and 40 inv(16) AML pts with 10 m DDX41-AML pts. JMP® Pro 14.1.0 Software was used for statistical analysis.
Results:
DDX41mutations characteristics: Our cohort included 19 (58%) myelodysplastic syndromes (MDS), 10 (30%) acute myelogenous leukemia (AML), 2 (6%) myeloproliferative neoplasms (MPN), one clonal cytopenia of undetermined significance (CCUS) (3%) and one (3%) germline carrier. Germline testing was carried out in 10 pts, 9 of whom (90%) were confirmed to be germline). The start-loss variant (p.M1I) was the most common mutation type (N=10, 31%). Other types were frameshift (N=9, 28%), missense mutation (N=8, 25%), nonsense (N=3, 9%), and splice site mutation (N=2, 2%). Twenty-one (65.6%) DDX41 mutations clustered in the N-terminus (NT), 7 (22%) in the helicase-C domain (HCD), and 4 (12.5%) in the DEAD-box domain. Compared to NT mutations, patients with HCD mutation had no family history of solid tumors and were more likely to have an accompanying additional DDX41-VUS (0% vs 70%; p=.001) and (N=6, 86% vs. N=2,10%; p=.0001); respectively.
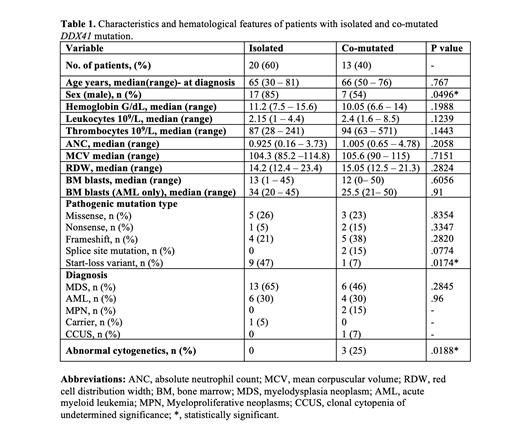
I solated vs. co-mutated DDX41: Twenty (60%) pts were isolated-DDX41 and 13 (40%) were co-mutated. The median DDX41-VAF was 48% vs. 45% (p= .2) in the isolated compared to the co-mutated cases, respectively. The median number of co-mutations in the 13 co-mutated cases was 1 (range,1-3) with DNMT3A (38%), ASXL1 (30%), JAK2 (N=3, 23%), and EZH2 (N=2, 15%) were the most common co-mutations detected. Isolated DDX41 had more males (85% vs. 54%, p=.05), the p.M1I variant (47% vs. 8%, p=.02), normal cytogenetics (100% vs. 91%, p= .02), and less family history of solid tumors (77% vs. 33%, p= .02) compared to their co-mutated counterparts. However, there was no difference in OS (p=.99). Comparison of clinical characteristics and hematological features of isolated and co-mutated DDX41 pts are reported in (Table 1).
Treatment and survival outcomes in DDX41-MDS/AML: Twenty-three (80%) patients were treated, MDS pts received hypomethylating agents (HMA) (N=10, 71%), HMA plus Venetoclax (HMA+VEN) (N=1, 7%), erythropoiesis-stimulating agents (N=2, 14%) and lenalidomide (N=1 ,7%). AML pts were treated with induction chemotherapy (N=6, 67%) and HMA+VEN (N=3, 33%). Overall response rate of MDS/AML patients was 77% and 100% of AML pts achieved complete remission (CR) when treated with induction chemotherapy or HMA+VEN regimen. There was no significant difference in OS between responders vs. non-responders 2-yr-OS (90% vs. 50%; p=.38) and treated vs. untreated 2-yr-OS (83% vs. 100%; p=.52).
Comparing m DDX41-AML vs. core binding factor-AML: After a median follow-up of 33.3 months, all m DDX41-AML patients were alive. There was a significantly better OS in mDDX41-AML patients compared to pts with t(8;21) AML with 2-yr-OS (100% vs. 51%; p=.024) and a trend of better survival when compared to inv(16) AML 2-yr-OS (100% vs. 84%; p=.2).
Conclusion
We describe the characteristics and outcomes of m DDX41 patients. We demonstrated that isolated and co-mutated m DDX41 patients have different features. Isolated DDX41 patients had male predominance, more p.M1I variant, normal cytogenetics and less family history of solid tumors. In this study we found that m DDX41 AML has high response to treatment and has comparable (if not possibly better) OS compared to other "favorable risk" AML. This study, although limited by the small number of patients, supports the universal testing for DDX41 mutation in adults with MN diagnosis.
Al-Kali: Astex: Other: Research support to institution; Novartis: Research Funding. Foran: abbvie: Research Funding; OncLive: Honoraria; boehringer ingelheim: Research Funding; trillium: Research Funding; pfizer: Honoraria; takeda: Research Funding; revolution medicine: Honoraria; bms: Honoraria; gamida: Honoraria; actinium: Research Funding; aptose: Research Funding; novartis: Honoraria; servier: Honoraria; taiho: Honoraria; syros: Honoraria; sanofi aventis: Honoraria; certara: Honoraria; kura: Research Funding; h3bioscience: Research Funding; aprea: Research Funding; sellas: Research Funding; stemline: Research Funding. Badar: Pfizer Hematology-Oncology: Membership on an entity's Board of Directors or advisory committees. Salama: Mayo Clinic: Current Employment, Other: Mayo Clinic had the contractual work for the central pathology review for this study and I was one of the reviewing pathologists; Constellation Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees. Litzow: Astellas: Research Funding; Biosight: Other: Data monitoring committee; Amgen: Research Funding; AbbVie: Research Funding; Actinium: Research Funding; Pluristem: Research Funding; Jazz: Other: Advisory Board; Omeros: Other: Advisory Board. Patnaik: Stemline Therapeutics: Membership on an entity's Board of Directors or advisory committees; Kura Oncology: Research Funding; Stemline Therapeutics: Membership on an entity's Board of Directors or advisory committees.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract